Advanced Cranial and Upper Cervical Instability Presentation in HSD/EDS
Presented by Patricia Stott
12-Month Subscription
Unlimited access to:
- Thousands of CE Courses
- Patient Education
- Home Exercise Program
- And more
This course explores the advanced clinical presentations of cranial and upper cervical instability (UCI) in individuals with hypermobility spectrum disorders (HSD) and Ehlers-Danlos syndromes (EDS), highlighting their unique anatomical, neurological, and connective tissue–related complexities. Clinicians will learn how abnormal connective tissue integrity in both the central and peripheral nervous systems contributes to a wide range of symptoms and overlapping diagnoses, such as functional seizures, intracranial pressure dysregulation, jaw dysfunction, and tethered cord syndrome. Emphasis is placed on identifying severity levels, evaluating signs and symptoms, and considering the body’s global pressure and neurological systems to guide care. Healthcare providers will gain practical tools for assessing moderate to severe cases and tailoring interventions based on a patient’s individual tolerance, often requiring work away from the cervical spine. This course is designed for physical therapists, athletic trainers, and rehabilitation professionals in outpatient neurological and orthopedic care settings who treat complex hypermobility cases.
Learning Objectives
- Consider the more common cranial issues in those with HSD/EDS
- Reflect on the associated connections between cranial and cervical spine issues and other pathologies
- Determine the severity of moderate to severe clinical presentations of upper cervical instability in HSD/EDS
- Formulate general treatment strategies and approaches to use in patients with moderate and severe upper cervical instability
Meet your instructor

Patricia Stott
Patricia Stott treats primarily those with HSD/EDS and those considered highly sensitive patients at her own practice, Elevation Wellness, outside the Denver metro area in Colorado. Also trained in functional and herbal medicine, she works on health and wellness through holistic strategies with these patients, both in person…
Chapters & learning objectives
1. Cranial Presentation in HSD/EDS
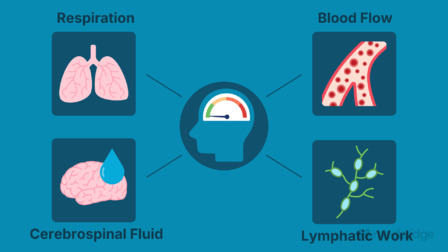
This chapter reviews the critical role of connective tissue in cranial and neurological health, examining how structural vulnerabilities in the brain’s extracellular matrix and blood–brain barrier affect neuroinflammation and function, or processing. Clinicians will learn about brain-specific pathologies seen in HSD/EDS populations, including functional seizures, the spiky-leaky theory of CSF regulation, and other additional correlated cranial diagnoses.

2. Associated Conditions With Cranial and Cervical Pathologies in HSD/EDS
Building on cranial concepts, this chapter explores how systemic pressure systems and fascial connections influence cranial and upper cervical symptoms. Topics include CSF leaks, Chiari malformation, cerebellar ectopia, tethered cord syndrome, and diaphragm dysfunction. Clinicians will develop a framework for recognizing how overlapping conditions compound instability and guide individualized treatment planning.

3. Upper Cervical Instability: Moderate and Severe Presentations
This chapter defines the clinical spectrum of moderate to severe upper cervical instability, with a focus on symptom provocation patterns, neurological involvement, and recovery responses. It details observation and movement assessments, including a qualitative look at proprioceptive testing, and provides guidance on classifying severity to shape appropriate treatment entry points and referral needs.
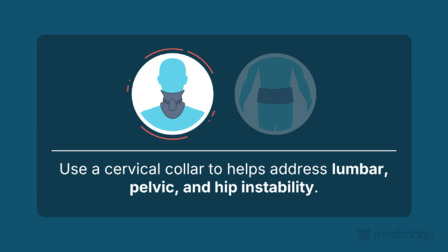
4. General Treatment Strategies for Cranial and Upper Cervical Advanced Presentations
Clinicians will learn to navigate treatment for highly reactive presentations by prioritizing autonomic regulation, core and pelvic stability, and remote interventions. The chapter outlines a tiered care model for addressing systemic contributors such as MCAS, intracranial pressure dysregulation, and jaw or airway involvement, emphasizing malleability, safety, and individualized care strategies.
More courses in this series
Advanced Cranial and Upper Cervical Instability Presentation in HSD/EDS
Patricia Stott

Advanced Upper Cervical Supportive Strategies With HSD/EDS
Susan Chalela and Patricia Stott
Advanced Upper Cervical Instability Direct Interventions in HSD/EDS
Susan Chalela and Patricia Stott